Understanding Noninvasive Prenatal Testing (NIPT)
Noninvasive prenatal testing (NIPT) for genetic conditions first became available in the United States in 2011. This new technology represents an incredible advance in our ability to screen for the most common chromosomal conditions. In recognition of this fact, the American College of Obstetricians and Gynecologists (ACOG) has recommended that providers offer NIPT to all pregnant people, regardless of their age or baseline risk for carrying a baby with a genetic condition.
Why Prenatal Genetic Screening?
Approximately 1 in 150 babies born in the United States has a chromosomal condition that can affect their health, growth, and development.4 These conditions occur at random due to errors in sperm or egg cells, so any baby can have a chromosomal condition, regardless of its parents or background.
What Are Chromosomes?
Our DNA contains genes, the instructions for how our bodies grow and function. Inside each of our cells, the DNA is packaged into tight bundles. These bundles are known as chromosomes.
Normally, humans have 23 pairs of chromosomes, 46 total. We inherit one set of chromosomes from each parent.6
What Are Chromosomal Conditions?
Sometimes a problem during the development of the egg or the sperm, a mistake during fertilization, or an early error in fetal cell division results in the baby receiving too many, too few, or extra or missing pieces of chromosomes. These errors are known as chromosomal conditions. Chromosomal conditions involve a change in the number of chromosomes or in the structure of a chromosome.7
Some examples of abnormalities in the number of chromosomes are:
-
Trisomy (an extra chromosome)
-
Monosomy (a missing chromosome)
-
Triploidy (an extra full set of chromosomes)
Some examples of abnormalities in the structure of a chromosome are:
-
Deletions (a missing piece of a chromosome)
-
Microdeletions (a missing piece of a chromosome too small to see with a microscope)
-
Duplications (an extra copy of a segment of a chromosome)
The most common chromosomal condition is trisomy 21 (Down syndrome), which occurs in approximately 1 in 700 live births in the United States,2 and accounts for 8-10% of severe genetic conditions.8 Down syndrome is caused by an extra full or partial piece of chromosome 21. 9
Other chromosomal conditions include trisomy 13 (Patau syndrome), trisomy 18 (Edwards syndrome), and sex chromosome conditions involving the X and Y chromosomes such as Turner syndrome and Klinefelter syndrome. 22q11.2 deletion syndrome, also known as DiGeorge syndrome, is a common microdeletion.
The risk for having a baby with certain chromosomal conditions, such as Down syndrome, increases with the age of the biological mother. But maternal age is only a risk factor. Genetic conditions primarily occur by random chance and cannot be predicted based on maternal age alone.10
For example, if only pregnancies involving a biological mother over the age of 34 received diagnostic testing with amniocentesis, the majority of Down syndrome cases would go undetected: 70% of Down syndrome cases occur in pregnancies involving biological mothers under age 35.11
In addition to maternal age, other risk factors include:12
-
Having a personal or family history of a genetic condition
-
Having had a child with a genetic condition
-
Having received a screening test or ultrasound that shows an increased risk of a chromosomal condition
What Is NIPT?
NIPT is a prenatal genetic screening test that requires only a simple blood draw from the pregnant person. It examines cell-free DNA (cfDNA) in the blood to assess a baby’s chance of having certain genetic conditions.
During the first trimester of pregnancy, the baby develops a placenta, an organ that connects it with the pregnant person’s blood supply. The placenta releases fragments of placental DNA into the pregnant person’s bloodstream. This placental DNA is usually identical to the baby’s DNA.
NIPT analyzes the placental DNA in the pregnant person’s bloodstream to screen for certain genetic conditions, such as trisomy 21 (Down syndrome), trisomy 13, and trisomy 18.
How Does NIPT Compare With Other Prenatal Screening?
Screening tests, including NIPT, are designed to help parents learn if their pregnancy is at a higher risk for health problems. Before NIPT was available, pregnant people could have other types of screening for genetic conditions, or they could undergo diagnostic testing with more invasive procedures.
Conventional screening methods combine ultrasound measurements with levels of hormones and proteins in the pregnant person’s blood to provide a risk estimate. Many different types of conventional screens are available, such as the sequential screen, first trimester screen, the quad screen, and the integrated screen. These screens are performed at different times during the first and second trimesters. Conventional screens have one major benefit: they are noninvasive, so they do not increase the risk of miscarriage.
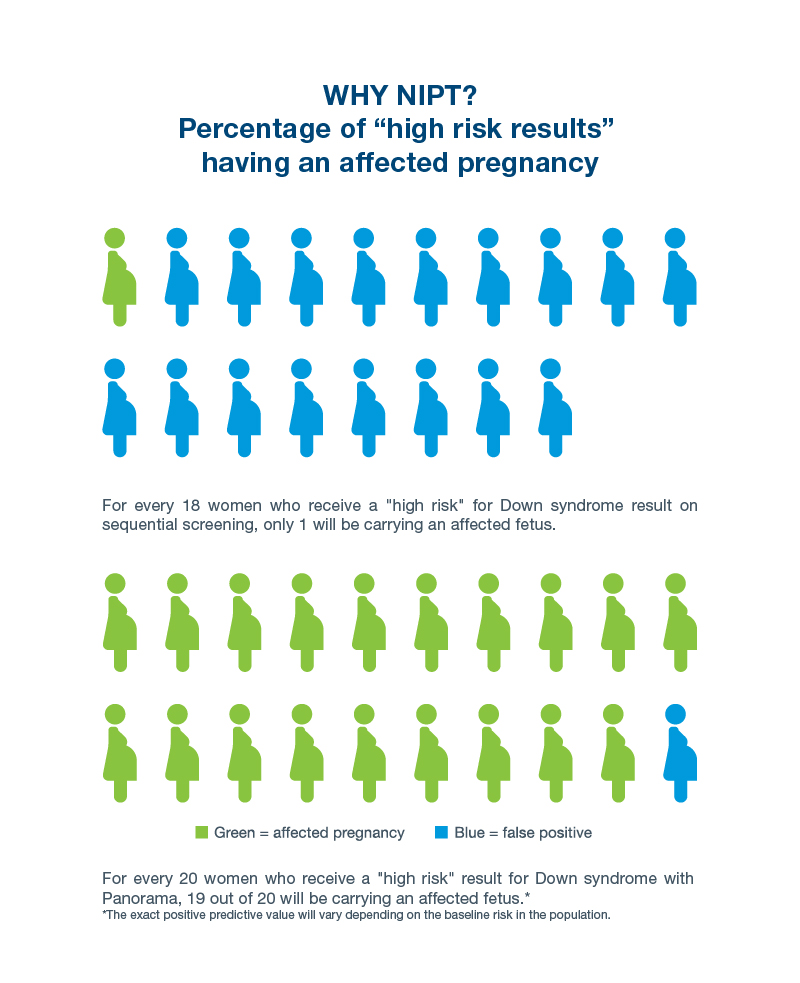
Conventional screening tests also have some major downsides. These screens raise a high number of false alarms: about 1 in every 20 pregnant people screened are identified as high risk. They also miss 1 in every 5-10 cases of Down syndrome, and have even lower detection rates for other, less common genetic conditions.4
The main value of NIPT is that it provides a much more reliable and accurate risk assessment than conventional screenings, without increasing the risk for miscarriage.How Does NIPT Compare to Diagnostic Testing?
Diagnostic tests are designed to determine with certainty whether the baby has a specific genetic condition. Their main advantage is exactly that: they provide a clear yes or no answer as to whether your baby has a genetic condition.
Two prenatal diagnostic tests are currently available: chorionic villus sampling (CVS) and amniocentesis. CVS can be performed by biopsying the placenta with a small plastic catheter or needle, and amniocentesis is performed by aspirating amniotic fluid with a needle.
Diagnostic tests also have drawbacks:
-
Limitations on timing: CVS is performed at the end of the first trimester, between 10-13 weeks gestation. Amniocentesis is performed in the second trimester, usually after 15 weeks gestation.13
-
A slightly increased risk of miscarriage: The increased risk of miscarriage is about 1 in 455 for CVS and 1 in 900 for amniocentesis.13
For these reasons, many people prefer to start with noninvasive screening tests that provide a risk assessment rather than a diagnosis, but that do not raise the risk of miscarriage.
After receiving a risk estimate from NIPT, pregnant people can use this information to decide if they want to have diagnostic testing.
When Is NIPT Performed?
Compared to diagnostic testing and conventional screens, NIPT has another advantage: timing. NIPT can be performed as early as nine weeks of pregnancy.14 In comparison, the most commonly used of the conventional screening methods, the sequential screen, does not provide a final risk assessment until the second trimester.15
Receiving information about their baby’s risk of having a genetic condition earlier gives pregnant people additional time to decide whether to pursue diagnostic testing, to discuss next steps with their clinicians or a genetic counselor, to identify pediatric specialists, and to update insurance coverage.16
How Accurate Is NIPT?
When evaluating screening test accuracy, researchers and physicians consider several aspects of test performance.
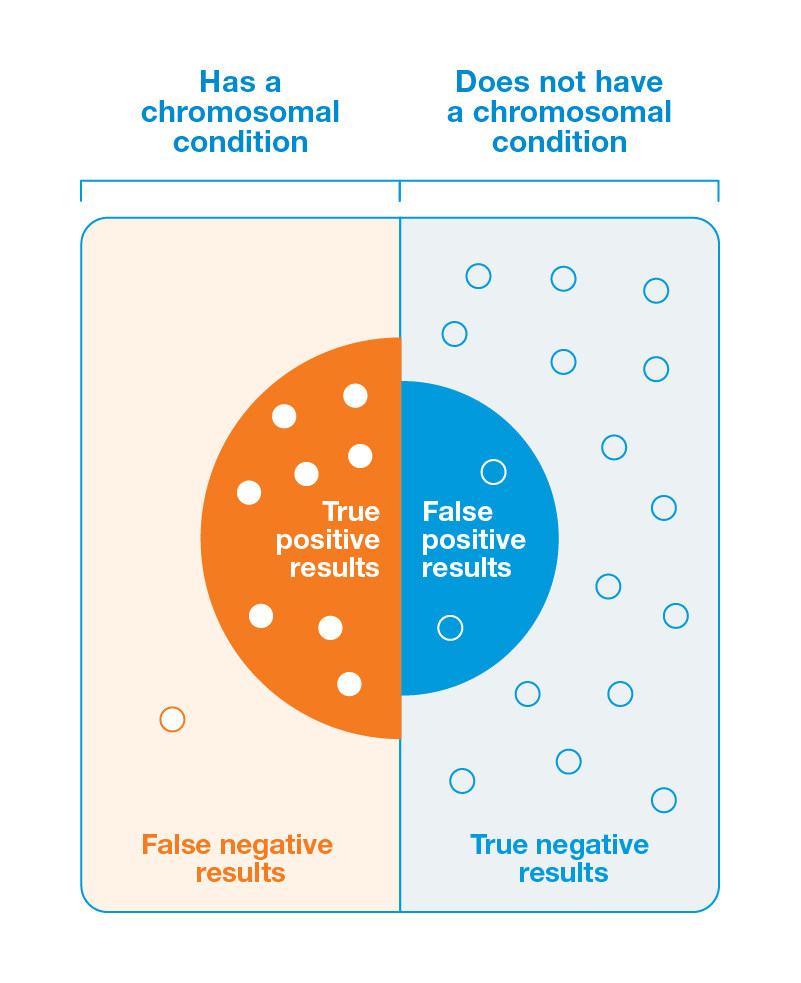
The first is sensitivity. Sensitivity refers to how often a pregnancy with a chromosomal condition correctly receives a positive result. Sensitivity tells us how many people with the condition are correctly identified as having it and sensitivity can help estimate the rate of false negatives.
The second is specificity. For prenatal screens, specificity refers to how often a pregnancy without a chromosomal condition correctly receives a negative result. Specificity tells us how many people without the condition are correctly identified as not having it and specificity can help estimate the rate of false positives.
Different conventional screens have differing sensitivities and specificities. The sequential screen for trisomy 21–which combines findings from ultrasound measurements, blood hormone levels, and protein markers taken in both the first and second trimesters–is the most accurate of the conventional screens. The final (second trimester) result of the sequential screen has a sensitivity of approximately 90% for detecting trisomy 21.16,17
NIPT screens are far more accurate than the sequential screen for many genetic conditions. For example, Natera’s NIPT, PanoramaTM, has a specificity of >99.9% and a sensitivity of >99% for trisomy 21.18
How Accurate Is NIPT for Determining Biological Sex?
Not only does NIPT provide information about specific genetic conditions, but it can also tell you the biological sex of your baby. In a recent study of over 1 million pregnancies, NIPT correctly determined fetal sex in over 99.99% of them.17
What Does a High Risk NIPT Result Mean?
Although NIPT screening tests are highly accurate, receiving a “positive” or “high risk” result does not mean that your baby definitely has a genetic condition. Despite a high degree of accuracy, NIPTs are screening tests and can have false positives.
How can the NIPT be both highly accurate and still return false positives? This apparent inconsistency occurs because the interpretation of a result depends not only on a screen’s sensitivity and specificity, but also on how frequently the condition being screened for occurs in the population being screened. This statement is true for all screening tests, not just NIPT. For example, seeing an unusual spot on a screening test like a mammogram does not necessarily mean a person has cancer—a diagnostic test like a biopsy is required to determine if cancer is present.
The rarer the condition being screened for during pregnancy, the more likely it is that a positive result will be a false positive. For very rare conditions, even highly specific and sensitive screens generate many “false alarms” (that is, false positives, or “high risk” results for pregnancies without a chromosomal condition). Other risk factors like parental age and family history also affect a person’s chances of a false positive.23
If you receive a “high risk” or “positive” screening result, diagnostic testing with CVS or amniocentesis is needed to determine if your result is a true positive. Speaking with a genetic counselor can also help you understand the implications of your result and decide on next steps.
Positive Predictive Value and Prenatal Screening Tests: An Example
The chance that a screen positive result correctly identifies a genetic condition, making it a true positive, is known as the screen’s positive predictive value, or PPV. A screening test’s PPV depends on the sensitivity and specificity of the screen itself, and on how common a particular condition is in a given population.
To see how positive predictive value (PPV) works in practice, let’s compare NIPT with the sequential screen regarding their abilities to detect trisomy 21, the genetic condition that causes Down syndrome.
After testing performed in the first and second trimester is completed and results are combined, the sequential screen misses approximately 1 in 20 cases of trisomy 21, and 17 in 18 of its positive results are false positives. 20
NIPTs have much higher sensitivity and specificity than even the most accurate of the conventional screens, the sequential screen. In other words, NIPTs miss fewer cases and have fewer false positives. For example, Natera’s NIPT, Panorama, misses fewer than 1 out of 100 cases of trisomy 21. Only 1 out of every 20 Panorama high risk results for trisomy 21 is a false positive.18
How Accurate Is NIPT for Detecting Other Genetic Conditions?
Because Down syndrome is the most common chromosomal condition, all prenatal screening tests, including NIPT, have higher accuracy for detecting Down syndrome than they do for detecting other, less common genetic conditions.
Most NIPTs screen for trisomy 21 (Down syndrome), trisomy 13 (Patau syndrome), and trisomy 18 (Edwards syndrome). Some also screen for sex chromosome conditions and specific microdeletions.
For example, in addition to Down syndrome, Panorama screens for:
-
Trisomy 13 and trisomy 18
-
Triploidy (three copies of every chromosome as opposed to the normal two)
-
Common sex chromosomal conditions such as Turner syndrome and Klinefelter syndrome
-
Some of the most common microdeletions (genetic conditions caused by small missing pieces of a chromosome), such as 22q11.2 deletion syndrome (DiGeorge syndrome); this test is optional.
According to the American College of Obstetricians and Gynecologists (ACOG), NIPT is the most accurate screen for these relatively common genetic conditions. But, even with NIPT, there is still a chance of receiving a false positive or a false negative. Diagnostic testing with CVS or amniocentesis is always recommended to determine if a positive result is a true positive.
Communication Is Essential
NIPT is much more accurate than conventional prenatal screens. However, it still only provides information about your risk of carrying a baby with a specific genetic condition. It is not a diagnostic test. It is important to discuss your NIPT results with your healthcare provider. You could also speak with a genetic counselor to discuss your results and next steps.
Similarly, receiving a low risk result means that your baby’s risk for specific genetic conditions is low. It is not a guarantee that your baby does not have those or other genetic conditions. NIPT and other screens test for a handful of the most common chromosomal conditions, but do not cover the full range of the over 10,000 human genetic conditions that have been identified.2 Many of these conditions are extremely rare and thus not screened for by NIPT or other prenatal screens.
As part of our commitment to our patients, we provide complimentary genetic information sessions with board-certified genetic counselors. Our counselors are available to answer questions from 6 AM to 5 PM Pacific Time, Monday through Friday, excluding holidays. Please call 866-985-4336 and ask to speak with the on-call genetic counselor. You may also email gc@natera.com with questions.
References
1Gadsbøll, K. et al. Current use of noninvasive prenatal testing in Europe, Australia and the USA: A graphical presentation. (2020). Acta Obstet. Gynecol. Scand. 99, 722–730.
2Centers for Disease Control and Prevention. Data & Statistics on Birth Defects. (2020).
3Centers for Disease Control and Prevention. What are Birth Defects? (2021).
4Carlson, L. M. & Vora, N. L. (2017) Prenatal Diagnosis: Screening and Diagnostic Tools. Obstet. Gynecol. Clin. North Am. 44, 245–256.
5Cuckle, H. & Maymon, R. (2016). Development of prenatal screening--A historical overview. Semin. Perinatol. 40.
6The American College of Obstetricians and Gynecologists. Genetic Disorders. (2021).
7National Institutes of Health: National Center for Advancing Translational Sciences. FAQs About Chromosome Disorders. (2017).
8Society for Maternal Fetal Medicine. Cell-Free DNA Screening. Retrieved January 10, 2022.
9National Down Syndrome Society. What is Down Syndrome? (2017).
10Hansen, J. P. (1986) Older maternal age and pregnancy outcome: a review of the literature. Obstet. Gynecol. Surv. 41, 726–742.
11Nicolaides, K. H. Screening for chromosomal defects. (2003). Ultrasound Obstet. Gynecol. 21, 313–321.
12The American College of Obstetricians and Gynecologists. Amniocentesis. (2021).
13UCSF Health. FAQ: Chorionic Villus Sampling (CVS). (2019).
14Natera Panorama FAQ. (2020).
15The American College of Obstetricians and Gynecologists. Prenatal Genetic Screening Tests. (2020).
16The American College of Obstetricians and Gynecologists. Prenatal Genetic Diagnostic Tests. (2020).
17Dhamankar, R., DiNonno, W., Martin, K. A., Demko, Z. P. & Gomez-Lobo, V. Fetal Sex Results of Noninvasive Prenatal Testing and Differences With Ultrasonography. (2020). Obstet. Gynecol. 135, 1198–1206.
18Dar P, et al. Cell-free DNA screening for trisomies 21, 18 and 13 in pregnancies at low and high risk for aneuploidy with genetic confirmation. (2022). Am J Obstet Gynecol. https://doi.org/10.1016/j.ajog.2022.01.019
19DiNonno, W. et al. Quality Assurance of Non-Invasive Prenatal Screening (NIPS) for Fetal Aneuploidy Using Positive Predictive Values as Outcome Measures. (2019). J. Clin. Med. Res. 8.
20Benn, P. A., Kaminsky, L. M., Ying, J., Borgida, A. F. & Egan, J. F. X. Combined second-trimester biochemical and ultrasound screening for Down syndrome. (2002). Obstet. Gynecol. 100, 1168–1176.
21Genetic AllianceUK. Genetic disorders. (2016).
22Dar P, Jacobson B, et al. Cell-free DNA screening for prenatal detection of 22q11.2 deletion syndrome. (2022). Am J Obstet Gynecol. Jan 13:S0002-9378(22)00006-0.
23Lutgendorf, MA & Stoll, KA. Why 99% may not be as good as you think it is: limitations of screening for rare diseases. (2016) J Matern Fetal Neonatal Med. 29:7, 1187-1189.
