Navigating the IVF Journey
Pursuing in vitro fertilization (IVF) is a personal decision. It’s one that is reached for many reasons, such as endometriosis, polycystic ovarian syndrome (PCOS), blocked fallopian tubes, low sperm count, use of donor egg or sperm, need or desire for surrogate pregnancy, or concerns about passing on a genetic condition.
Whatever your reason for considering IVF, it is the most common and effective type of assisted reproductive approach available,1 helping more than 8 million people around the world realize their dreams of having a baby.2
While the IVF process involves complex treatments and procedures, many technologies, including genetic testing, can help increase your chance for success.
Your Initial Consultation
During your initial consultation, you will meet with a reproductive endocrinologist (REI), an OBGYN with at least three years of additional training in reproductive hormones and infertility. You could be asked to bring your medical records, including any records from prior fertility treatment, and your insurance information.
During the visit, the doctor will review your medical history, assess you and your partner’s overall health, and ask detailed questions about previous efforts to conceive. They could ask about lifestyle factors that can affect fertility such as smoking and alcohol use, and they will review your family’s history of medical and genetic conditions.
You will have time to ask questions about the process, the clinic’s success rates, and any other concerns you could have. This first visit can be a stressful and exciting time, so consider taking notes to help you keep track of all the information you receive.
Bloodwork and Checkup
The initial consultation will usually involve various tests:
Female testing:
-
A transvaginal ultrasound to look at your uterus and ovaries
-
Blood work:
-
FSH (follicle stimulating hormone)
-
LH (luteinizing hormone)
-
Estradiol
-
TSH (thyroid stimulating hormone)
-
PRL (Prolactin)
-
Infectious disease screening
Male testing
-
Semen analysis
-
Blood work
-
Infectious disease screening
-
Possible hormone evaluation
During your initial appointment, next steps will be discussed which may include additional tests for you and/or your partner, such as a hysterosalpingogram (HSG) to determine if your fallopian tube(s) are blocked. These are the tubes where in vivo (inside body) fertilization takes place and transports the egg/early embryo to your uterus for implantation.
Your treatment plan and the costs associated with various procedures are also usually shared with you. Some clinics may have an on-staff financial counselor who can help you understand your insurance coverage and walk you through different payment plans.
Carrier Screening for You and Your Partner
Carrier screening is a genetic test to determine whether you and your partner are at risk for passing on an inherited genetic condition, such as cystic fibrosis or spinal muscular atrophy, to your child. Regardless of the method used to conceive, the American College of Obstetricians and Gynecologists (ACOG) recommends that carrier screening be offered to all people who are planning to get pregnant or who are pregnant if they have not been screened previously.3 Undergoing carrier screening prior to attempting pregnancy provides knowledge about your carrier status which may affect your choices in your treatment plan.
How Does Carrier Screening Work?
Carrier screening looks for genetic changes that can affect how a gene works. Humans carry two copies of most of their genes. While there are different ways that genetic conditions can be passed down or inherited in families, carrier screening tests for genetic conditions that happen when both copies of a gene pair have a mutation. These are called recessive genetic conditions. A carrier of a recessive genetic condition is someone who has a mutation in one of the genes in a pair. A couple can have a child with a recessive condition when both the mother and the father are carriers of the same condition.
All of us are carriers of at least one genetic condition. Most carriers are healthy and have no family history of the genetic condition they carry or understanding of how that condition could impact their child. Carrier screening is a type of test that allows you to determine your risk for passing an inherited genetic condition to your child.
Carrier screening also looks for certain genetic conditions, called X-linked conditions, such as Duchenne muscular dystrophy and fragile X syndrome. When the biological mother is a carrier of one of these conditions, her male children have a 1 in 2 chance of inheriting the mutation and developing the condition. Female children typically will not develop the condition, but they will have a 1 in 2 chance of being carriers.
Some couples who are carriers of the same recessive condition or the female carrier of an X-linked condition may opt to pursue IVF with preimplantation genetic testing (PGT). PGT identifies embryos that are unaffected, affected, or may be found to be a ‘carrier’ embryo. The goal is to identify unaffected or carrier embryos from affected for future transfer decisions and to improve the chance of a healthy pregnancy.
Natera offers the Horizon carrier screen for anyone who is planning to conceive or currently pregnant, and the Spectrum preimplantation genetic test (PGT) for people pursuing IVF. Additionally, for people who are concerned about their genetic risk for certain cancers that can be inherited, there is a test called the Empower hereditary cancer test.
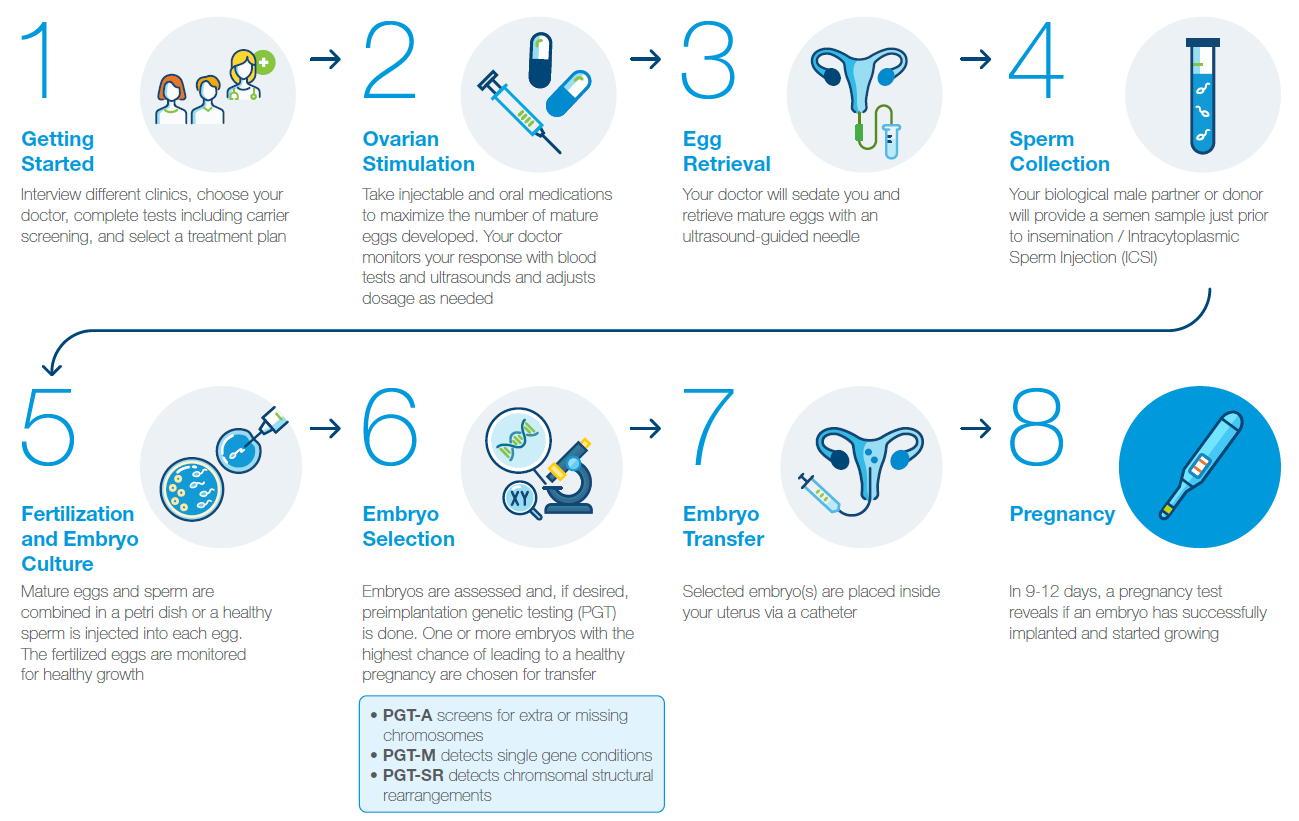
During IVF, ovarian stimulation is used to help you produce as many mature eggs as possible, increasing the chance for fertilization and achieving pregnancy. The process requires taking medications to optimize your ovulation cycle, including injectable hormones that stimulate egg maturation.
During a typical menstrual cycle, immature eggs develop inside fluid-filled cysts known as follicles. With each cycle, many follicles begin to develop in the ovaries, but usually only one, the dominant follicle, goes on to contain a mature egg which is released during ovulation.
The goal of follicle stimulation is to encourage more eggs to reach maturity for retrieval. Follicle stimulation involves receiving three different types of medication:
-
A medication to suppress ovulation from occurring, either a gonadotropin releasing hormone agonist (GnRH-agonist) or a GnRH-antagonist
-
A follicle stimulating hormone (FSH) that stimulates the development of multiple mature follicles and eggs
-
A ‘trigger shot’, often human chorionic gonadotropin (HCG), resulting in final maturation of the eggs
These medications are usually taken on a daily basis at set times and are an important part of the IVF cycle. The hormones can also impact your mood. Go easy on yourself.
During this process, your doctor will closely monitor the hormone levels in your blood and use ultrasound to assess follicle development. Depending on your body’s response, they could adjust your medication dosage, as everyone responds to these hormones differently. Too high of a dose can cause ovarian hyperstimulation syndrome, a potentially serious side effect, which can lead to enlarged ovaries, pain, and bloating.
Gamete is the scientific name for egg and sperm cells—special cells that are combined (fertilized) in hopes to become an embryo. Egg retrieval is the procedure for extracting the eggs from your ovaries and placing them into a test tube. First, you will be sedated. Then your vagina will be washed with a fluid, and your doctor will insert an ultrasound-guided needle through your vagina into your ovaries to extract mature eggs. The procedure usually takes 15-60 minutes. Afterward, you will be moved to another room to rest for approximately an hour.
Because of the sedation you received, you will need to take the day off work and have someone available to drive you home. To avoid straining your abdomen, you will also need to avoid strenuous exercise and heavy lifting for a few days.
Rarely, egg retrieval can cause side effects, such as infection, injury and bleeding.
If you’re planning to use sperm from your male partner or a donor, they will need to provide a sample. Different clinics have different recommendations for how long to abstain from ejaculation prior to sample production—usually 2-5 days is recommended. The sample is usually collected by masturbation.

Fertilization
There are two common methods of fertilization used in IVF:
-
Conventional fertilization. The egg and sperm cells are mixed together in the lab and incubated overnight.
-
Intracytoplasmic Sperm Injection (ICSI). A single healthy sperm is selected and injected into each egg. ICSI is most often used in cases of low sperm count or low sperm motility (movement), or to boost success rates after previous failed IVF attempts. ICSI is also recommended if PGT testing is being performed to avoid sperm contamination on the embryo samples.
Embryo Culture
After fertilization, the egg divides into a two-cell zygote. These cells continue to duplicate and divide over the next three days. This phase is known as the cleavage stage.
Once 16 cells are present, the zygote enters the morula stage. During the morula stage, the cells arrange themselves into a hollow circle in preparation for becoming a blastocyst.
On day 5 or 6, the zygote becomes a blastocyst. The blastocyst contains two cell layers: an outer layer or shell which will become the placenta and amniotic sac and an inner layer which will develop into the baby. The inner cells continue to divide and push against the outer layer of cells, eventually breaking the outer shell (a process known as “hatching”), which prepares the blastocyst for implantation.
Prior to implantation, your clinic will grade your embryos by looking at them under a microscope and assessing their cells’ shape, size, and structure. Grading is done on day 3 or day 5 of embryo development. The exact criteria used for grading depends on when the grading is performed.
After grading, embryos can be transferred or biopsied for PGT and/or frozen for potential later use.
Embryo selection is used to help increase the chance of a healthy pregnancy and baby. Your doctor will monitor growing embryos for signs of expected development and could recommend PGT to screen for genetic conditions that aren’t visible under a microscope.
What is Preimplantation Genetic Testing (PGT)?
Even embryos that look good under a microscope can have genetic abnormalities that affect their ability to implant and lead to a healthy pregnancy. PGT can help promote IVF success by assessing embryos for different types of genetic conditions, including:
-
Extra or missing chromosomes (PGT-A)
-
Single gene conditions (PGT-M)
-
Structural rearrangements (PGT-SR)
PGT can help your doctor select the embryos with the highest chance for a healthy pregnancy, birth, and baby.
Common reasons for considering PGT-A include:
-
Being over 35 years of age
-
Having had a prior pregnancy or child with a genetic or chromosomal condition
-
Having repeated IVF cycles without becoming pregnant
-
Having multiple pregnancy miscarriages
-
Planning on a single embryo transfer
Common reasons for considering PGT-M or PGT-SR include:
-
Knowing that parents are at risk of having a child with an inherited genetic condition
-
Knowing that one parent has a structural chromosome rearrangement
Will it delay my IVF cycle?
PGT requires removing 3-8 cells from the outer layer of the blastocyst, the part of the embryo that will eventually develop into the placenta. The DNA of these cells is then screened for certain genetic conditions.
Because it can take a week or more to receive your results, it is normal for all tested embryos to be frozen for transfer at a later time. This process means that you cannot do a fresh embryo transfer and will have to wait until your next cycle to transfer a frozen embryo.
There are some additional benefits to delaying the transfer. During fresh embryo transfer, the hormones you took to stimulate egg maturation can affect your uterine lining and lower the chances of implantation. Fresh embryo transfer is also associated with a higher risk for certain complications such as ovarian hyperstimulation syndrome.6 For these reasons, some centers recommend frozen embryo transfer regardless of whether PGT is performed.
What is the success rate?
The success rate with PGT depends on a number of factors, including your age, the cause of infertility, and how many healthy embryos you have. For women over 35, PGT has been shown to lower miscarriage rates and to raise per transfer pregnancy rates.7,8 You should ask your IVF clinic about their success rates for pregnancy and live births when using PGT.
How accurate is PGT-A?
PGT-A is not 100% accurate. One reason for this less than perfect accuracy is mosaicism—when some of the embryo’s cells have the correct number of chromosomes and others do not. Because of mosaicism, noninvasive prenatal testing (NIPT) during pregnancy is still recommended, even if you have PGT. NIPT is a common screening test for chromosomal conditions that only requires a blood draw from the pregnant individual.
How is PGT performed?
PGT requires taking a small biopsy of cells from the growing embryo to perform genetic testing. Very early in embryo development, cells begin segmenting into two categories: cells that will become the fetus and cells that will become the placenta. When performing a biopsy for PGT, cells are removed from the part of the embryo that will become the placenta. While there is a small risk of damage to an embryo, as PGT biopsy techniques have become standardized, this risk has become minimal.
How much does it cost?
The cost of PGT varies from center to center and depends on the number of embryos being tested. It is best to speak with your IVF clinic regarding the cost of IVF, medications, and PGT.
What are the types of PGT?
Preimplantation Genetic Testing for Aneuploidy (PGT-A)
Regardless of how a pregnancy is conceived, the most common cause of miscarriage is chromosomal anomalies. Chromosomes are the structures that hold our DNA. Humans usually have 23 pairs of chromosomes, one set from each parent, for 46 total. Small errors during the formation of an egg or sperm, fertilization, or early embryonic growth can lead to extra or missing chromosomes or pieces of chromosomes. When this occurs, it is called aneuploidy.
PGT-A screens for aneuploidy in embryos produced through IVF.9 It is often recommended when the eggs used for IVF come from someone over age 35, as aneuploidy rates increase with age. PGT-A helps identify embryos that are most likely to result in a successful pregnancy.8
Spectrum PGT-A can reduce the time to pregnancy during IVF, increase pregnancy rates regardless of parental age, and reduce the chance of miscarriage. The test can also determine the biological sex of an embryo. For parents with additional genetic concerns, Spectrum PGT-A can be performed with PGT-M or PGT-SR using a single biopsy.
What is mosaicism & can PGT-A detect it?
Mosaicism is a condition in which some of an embryo’s cells have the expected 46 chromosomes and other cells have aneuploidy. It is caused by an error during cell division after fertilization. Depending on the type of aneuploidy in the mosaic cells and what proportion of cells are affected, it can lead to miscarriage or cause health conditions during pregnancy and after birth.
Mosaicism detection requires the use of NGS technology. Spectrum PGT-A has this capability. Spectrum can only detect mosaicism if the biopsied cells include both normal and aneuploid cells.
Preimplantation Genetic Testing for Single Gene/Monogenic Conditions (PGT-M)
Some genetic conditions, such as cystic fibrosis or sickle cell anemia, are caused by inherited genetic changes in one gene—this is why they are often called single gene conditions or monogenic conditions. Many of these conditions are known as autosomal recessive conditions—meaning for a baby to potentially inherit the condition, both parents must carry a change in the same gene.
Other single gene conditions, such as Huntington’s disease, only require inheriting one copy of a genetic change within a gene to develop the condition.
PGT-M tests for single gene conditions in embryos created through IVF.9 It can help parents select healthy embryos if they are worried about passing on a genetic condition to their children.
With Spectrum, PGT-A and PGT-M can be combined for more results from a single biopsy.
Preimplantation Genetic Testing for Structural Rearrangements (PGT-SR)
Structural rearrangements occur when a person has all the expected parts of their chromosomes, but some pieces are in different places than usual. For example, a segment of a chromosome could be upside down, but fully intact. Or the end of one chromosome could be swapped with the end of another. A person who carries a structural rearrangement usually does not have any health problems and is typically unaware that they are a carrier.
Issues with structural rearrangements generally only arise once someone starts trying to have children. Since pieces of their chromosomes are in atypical positions, when their gametes (egg or sperm) combine during fertilization, the chromosomes don’t always line up correctly. This misalignment means that their embryos are at much higher risk for chromosomal anomalies that can lead to infertility, miscarriage, and/or a child affected with a chromosomal condition.
PGT-SR tests for structural rearrangements in embryos produced through IVF.9 It is recommended for people who know that they have a structural rearrangement and want to select embryos that have the best chance of leading to a healthy pregnancy.
To offer more information when selecting the healthiest embryos for implantation, Spectrum can perform PGT-A and PGT-SR on a single embryo biopsy.
Transferring an embryo or embryos is the final step in the IVF process. Your doctor could prescribe progesterone supplements or other medications to help your body prepare for implantation. If you are using frozen embryos, they will be thawed before transfer.
The embryo transfer usually does not require any sedation. Your doctor will insert a catheter through your cervix into your uterus and use ultrasound to guide the placement of the embryo(s) along your uterine lining. You could be asked to have a full bladder during the procedure, as that can help make the ultrasound image clearer.
NIPT
PGT is a highly accurate tool for selecting healthy embryos for implantation, but it cannot rule out every potential genetic condition. Even if you have had PGT, many doctors still recommend standard prenatal testing once you are pregnant to help identify any health concerns early.
Noninvasive Prenatal Testing (NIPT) is a screening test that detects common chromosomal conditions early in pregnancy. It can help you and your doctor decide if further testing is necessary to rule out or diagnose a potential condition. NIPT analyzes your baby’s DNA with a standard blood draw from the pregnant individual and carries no increased risk to the pregnancy. Since NIPT offers greater accuracy than previously available noninvasive tests, ACOG supports offering NIPT for all pregnancies.10
Panorama NIPT is the most frequently ordered NIPT by physicians, with over 3 million patients served and counting.11Panorama’s unique SNP-based technology analyzes the 1% of DNA that makes us different, so it is the only NIPT capable of distinguishing your DNA from your baby’s, detecting maternal atypical genetic findings, and providing unique twins differentiation in a twin pregnancy.10,11,12
Your doctor could also recommend diagnostic testing such as chorionic villus sampling or amniocentesis to assess your baby’s health.
Your Partner in Prenatal Genetic Testing
IVF can be a long and complex process, but genetic testing can help support your path to a healthy baby. Natera is committed to improving access to genetic testing for every patient that could benefit. We offer broad in-network coverage, financial assistance programs, and price transparency across our tests.
As part of Natera’s commitment to our patients, we also offer complimentary genetic information sessions with board-certified genetic counselors before and after testing.
Disclaimer
The tests described have been developed and their performance characteristics determined by the CLIA-certified laboratory performing the test. The tests have not been cleared or approved by the US Food and Drug Administration (FDA). Although FDA is exercising enforcement discretion of premarket review and other regulations for laboratory-developed tests in the US, certification of the laboratory is required under CLIA to ensure the quality and validity of the tests. CAP accredited, ISO 13485 certified, and CLIA certified. © 2022 Natera, Inc. All Rights Reserved.
References
1Medline Plus. Assisted Reproductive Technology. Accessed March 18, 2022.
2Fauser B. Reproductive biomedicine online. 2019;38(2),133-137.
3ACOG Committee Opinion, Number 691. Carrier Screening for Genetic Conditions. Obstet Gynecol. 2017;129(3):e41-e55.
4Yang et al. BMC Pregnancy Childbirth. 2020;20,559.
5Gadson et al. Fertil Steril. 2020;114(3).
6Roque et al. Hum Reprod Update. 2019;25(1):2-14.
7Practice Committee of the American Society for Reproductive Medicine. Fertil Steril. 2012;98(5):1103-11.
8Viotti M. Genes (Basel). 2020;11(6):602.
9ACOG Practice Bulletin, Number 226. Screening for Fetal Chromosomal Abnormalities. Obstet Gynecol. 2020;136(4):e48-e69.
10Norwitz et al. J Clin Med. 2019;8:937.
11Hedriana et al. Prenat Diagn. 2020;40(2):179-184.
12Martin et al. Am J Obstet Gynecol MFM. 2020;2:100152.
