What is PGT-A? And How Does It Support IVF?
In vitro fertilization (IVF) is a medical procedure that has helped many people become parents. During IVF, eggs are collected and fertilized in a laboratory setting. The resulting embryos are then transferred into the uterus for implantation. If you are pursuing or considering IVF, you have likely heard that genetic testing can help increase the likelihood of a healthy pregnancy.
Genetic testing can be done at several points in the IVF journey. In this article, you’ll learn about one type of preimplantation genetic testing (PGT), which is done on a sample from an embryo before it is transferred to the uterus. PGT can help increase the likelihood that IVF will be successful by informing which embryos are most likely to be genetically healthy.
We’ll focus on the most common form of PGT: preimplantation genetic testing for aneuploidy (PGT-A). PGT-A looks at embryos to determine if they are likely to be affected by a chromosomal anomaly, which can have significant effects on a pregnancy and a baby.
What is a Chromosomal Anomaly?
Our DNA contains genes, the instructions for how our bodies grow and function. Inside each of our cells, our DNA is packaged into tight bundles called chromosomes. A human cell usually contains 23 pairs of chromosomes.1 We inherit half of our chromosomes from one biological parent and the other half from the other biological parent.
A chromosomal anomaly is a change in the expected number or structure of chromosomes. During reproduction, small errors in the formation of an egg or sperm, or in early embryo growth, can result in chromosomal anomalies. These errors can happen by random chance and can occur in all types of pregnancies, regardless of how they were conceived.2
What is Aneuploidy?
The most common chromosomal anomaly is called aneuploidy.3 Aneuploidy means a cell has extra or missing chromosomes, resulting in too much or too little genetic material that can seriously affect a baby’s development. Aneuploidy is the most common cause of miscarriage and occurs in about half of miscarriages.4
Some types of aneuploidy include:
-
Trisomy (an extra chromosome)
-
Monosomy (a missing chromosome)
-
Triploidy (an extra full set of chromosomes)
Each type of aneuploidy can have significant effects on an embryo’s chance of developing into a healthy pregnancy. Triploidy, while rare, can cause a developing baby to have severe growth problems.5 Most cases of triploidy result in early miscarriage.5 If a baby is born with triploidy, they are unlikely to survive more than a few days and will usually require major medical care.6
Aneuploidy is also the most common reason that an IVF cycle does not result in a healthy pregnancy. The likelihood of an embryo having aneuploidy increases with the biological mother’s age.7 Women under 35 years old have up to a 37% chance of aneuploidy being present in an embryo, and women over 40 years old have a 75% chance.7
What is PGT?
PGT is a form of genetic testing that looks at the genetic health of embryos produced during IVF. PGT screens embryos from an IVF cycle for certain genetic anomalies. Testing identifies which embryos have the highest chance of leading to a healthy pregnancy.
While PGT is highly accurate, it cannot detect every possible genetic anomaly. For that reason, if you become pregnant with an embryo that has been tested with PGT-A, your doctor will likely recommend standard prenatal testing to help identify any health concerns early.8
There are three types of PGT. Each type looks for different types of changes in an embryo’s genetic structure:
-
PGT-A (aneuploidy): extra or missing chromosomes
-
PGT-M (monogenic): certain changes in single genes
-
PGT-SR (structural rearrangements): certain changes in the structure of chromosomes
All three types of PGT are performed at the same stage of embryo development and can sometimes be performed on the same sample of cells.
Deciding whether to have PGT and which type(s) to have is an important step in your IVF journey. The decision can depend on your personal or family history. For example, if you know that you or your biological partner are carriers for a single-gene condition such as cystic fibrosis, you could opt for PGT-M.
PGT could also be a good choice for you if you simply want to know as much about your embryos as possible before transfer. Discuss your goals and questions with your doctor and/or genetic counselor before deciding on PGT and the specific types you want performed.
What is PGT-A?
PGT-A looks specifically at whether an embryo has aneuploidy—extra or missing chromosomes. Aneuploidy is a leading cause of embryo transfers that do not lead to implantation and pregnancy.7 Having PGT-A results can help your doctor choose the most genetically healthy embryo(s) to transfer.
You will sometimes see PGT-A referred to as PGS (preimplantation genetic screening). PGS is simply an older term for PGT-A. It reflects the fact that PGT-A is a screening test that provides the likelihood that embryos are affected by aneuploidy. It is not a diagnostic test. That is, PGT-A cannot tell you with absolute certainty whether an embryo has a chromosomal anomaly. However, today’s PGT-A methods are highly accurate for detecting the likelihood of an anomaly.
It’s important to understand that, as with any screening test, there is a possibility of false positive or false negative results with all types of PGT, including PGT-A. A false positive result on a PGT-A test means that the test reported a chromosomal anomaly when there was none. A false negative result on a PGT-A test means that a chromosome anomaly was not reported, but an anomaly is present in the embryo. The likelihood of a false positive or false negative result is small, and for many people does not outweigh the benefits of testing.
For some people, PGT-A has been shown to reduce the time to pregnancy.9 If your doctor recommends a single embryo transfer (SET) to avoid the possibility of a multiple pregnancy, PGT-A can help increase your confidence that you are choosing the embryo with the highest chance of developing into a healthy pregnancy.7 PGT-A has also been shown to decrease the chance of miscarriage.10
Who Should Consider PGT-A?
PGT-A is available to most people pursuing IVF. The decision whether or not to use PGT-A is up to you and your doctor. Your doctor is more likely to recommend PGT-A if you:
-
Are over the age of 35
-
Had a prior pregnancy or child with a genetic or chromosomal condition
-
Had repeated IVF cycles without becoming pregnant
-
Had multiple miscarriages
-
Are planning a single embryo transfer
Clinical studies suggest that PGT-A is especially useful if the egg provider is over 35 years old.7 The following graph illustrates how the rate of chromosomal anomalies increases with the age of the biological mother.7 These embryos were tested with SpectrumTM, a PGT-A from Natera.
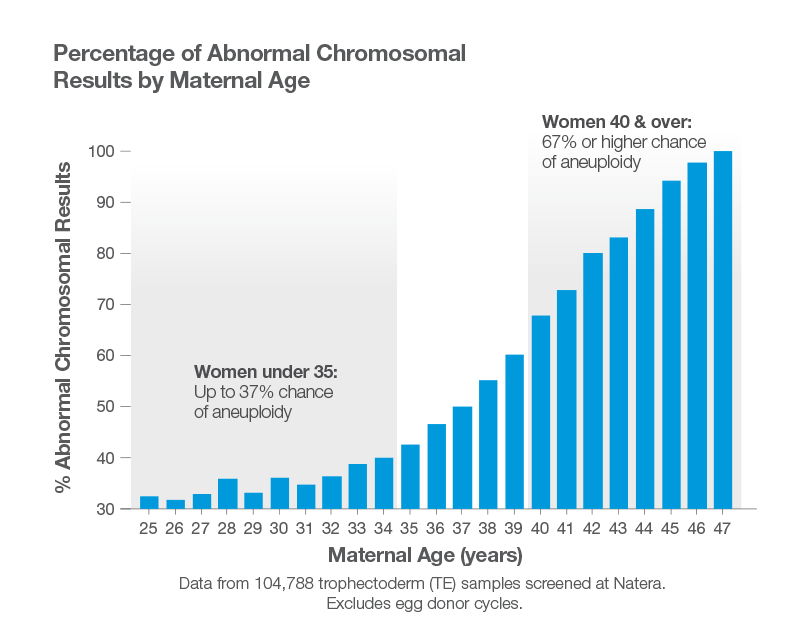
More than half of embryos provided by a biological female older than 37 had a chromosomal anomaly.7 For this reason, PGT-A is more likely to be recommended when the egg provider is older.
How Does PGT-A Work?
The PGT-A process usually begins 5-6 days after an egg is fertilized with sperm to form an embryo.11 At this stage, the embryo is known as a blastocyst. It contains 50-150 cells, some of which will become the fetus and some of which will become the placenta.12 Only cells that will develop into the placenta are collected for PGT-A testing. Using these cells reduces the chance that the cells that will develop into the fetus will be affected during the testing process.
First, a clinician carefully takes a small sample of cells—also known as a biopsy—from each embryo you want to be tested with PGT-A. PGT-A techniques have been refined to reduce the possibility of any damage to the embryo during the biopsy.13
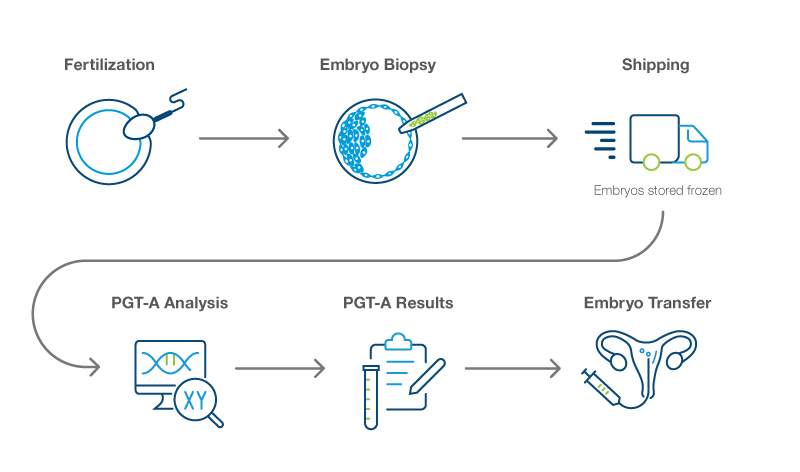
After the embryo sample is collected, it is shipped to the genetics laboratory that will perform the PGT-A. The embryos are then frozen and stored at the IVF clinic.
The genetic lab uses advanced technology to complete PGT-A on the cell samples it receives. The results will be sent to your doctor, who will review them with you. Your PGT-A report will inform you whether each tested embryo is likely to have aneuploidy (extra or missing chromosomes) or euploidy (the expected 46 pairs of chromosomes). If an embryo is identified as having aneuploidy, the affected chromosome and the type of aneuploidy are also reported.
After you discuss your PGT-A results with your doctor, you can decide if you’d like to transfer any of the embryos that were tested. You can choose to keep the embryos that you do not transfer frozen for later use.
To prepare your body for embryo transfer, your doctor will prescribe medications that thicken the lining of your uterus. In about 2-3 weeks, your doctor will thaw and transfer the selected embryo(s). Your doctor will schedule a pregnancy test about 12-14 days after the transfer to see if the embryo transfer has resulted in pregnancy.
PGT-A adds other considerations to your IVF cycle. For example, PGT prevents the possibility of a fresh transfer because embryos must be frozen while you wait for your PGT-A results. However, fresh transfers are not recommended for all people. In a fresh embryo transfer, the medications taken to encourage egg maturation can have effects on the lining of the uterus, and reduce the chance that a transferred embryo will implant. Fresh transfers are also associated with a higher likelihood of certain pregnancy complications.14 Since 2008, a higher rate of live deliveries has been noted in frozen cycle transfers, which can use PGT-A, compared to fresh cycle transfers, which cannot.15
Ultimately, the decision to use PGT-A is highly personal. You should talk with your doctor and/or genetic counselor to help you decide whether it is right for you.
Comprehensive PGT-A with SpectrumTM
Spectrum™ PGT-A from Natera has been studied to learn whether it helped people achieve their goal of a healthy pregnancy. Study results showed that PGT-A improves pregnancy rates for parents of all ages.7 Spectrum uses advanced genetic technology to screen all 24 chromosomes in a cell (22 chromosome pairs and the sex chromosomes X and Y).
Spectrum uses advanced sequencing technology to analyze embryo DNA. While it cannot confirm the parents of an embryo to prevent a mix up, it is able to detect a condition called mosaicism that can impact IVF success.
Mosaicism is a condition in which some of an embryo’s cells have the expected 46 chromosomes and other cells have aneuploidy. Mosaicism is caused by errors during cell division as an embryo grows. Depending on the type of aneuploidy in the mosaic cells and what proportion of cells are impacted, mosaicism can lead to miscarriage or cause health problems during pregnancy and after birth.16
Mosaicism detection requires adding the use of next generation sequencing technology. If you are concerned about the potential for mosaicism, Spectrum PGT-A can detect the condition as long as the biopsied cells contain both cells with the expected number of chromosomes and cells with aneuploidy. Talk with your doctor to learn if choosing Spectrum for mosaicism is best for you.
Getting the Most Out of PGT-A
If you’re curious about PGT-A, your doctor and/or genetic counselor can help you decide whether it can help you. If you have already received PGT-A and have questions about your results and what they mean, please discuss them with your doctor and/or genetic counselor.
A genetic counselor can help you make more informed decisions regarding PGT-A and other genetic tests. In some cases, your doctor will refer you for genetic counseling. If your doctor does not have a preferred genetic counselor or services are unavailable in your community, virtual genetic counseling services are available through many providers.
If you become pregnant, additional prenatal genetic testing options are available. These options include both screening and diagnostic tests, which can help you learn more about the genetic health of your developing baby.
As part of Natera’s commitment to our patients, we offer complimentary genetic information sessions with board-certified genetic counselors before and after testing.
Disclaimer
Spectrum tests have been developed and their performance characteristics determined by the CLIA-certified laboratory performing the test. The test has not been cleared or approved by the US Food and Drug Administration (FDA). CAP accredited, ISO 13485 certified, and CLIA certified. © 2022 Natera, Inc. All Rights Reserved.
References
1The American College of Obstetricians and Gynecologists. Genetic disorders: Frequently asked questions. Accessed March 17, 2022.
2National Human Genome Research Institute. Chromosome abnormalities fact sheet. Accessed March 17, 2022.
3Genetic Alliance; District of Columbia Department of Health. 2010 Feb 17. Appendix H, Chromosomal Abnormalities.
4Gu et al. Front Genet. 2021;12:667697.
5National Center for Advancing Translational Sciences. Triploidy. Accessed March 17, 2022.
6Walsh R, Sharma A. BMJ Case Reports CP. 2022;15:e244551.
714,988 TE samples screened at Natera
8The American College of Obstetricians and Gynecologists. Preimplantation genetic testing. Accessed March 17, 2022.
9Greco et al. Int J Mol Sci. 2020;21(12):4381.
10Forman et al. Hum Reprod. 2012;27:1217–22.
11Niu et al. Reprod Biol Endocrinol. 2020;18(4).
12StatPearls. Embryology, Week 1. Accessed March 17, 2022.
13Homer H. Aust N Z J Obstet Gynaecol. 2019;59(2):317-324.
14Yang et al. BMC Pregnancy Childbirth. 2020;20,559.
15Society for Assisted Reproductive Technology. More deliveries. Accessed March 17, 2022.
16StatPearls. Genetics, Mosaicism. Accessed March 17, 2022.
