Getting Started with the Empower Hereditary Cancer Test
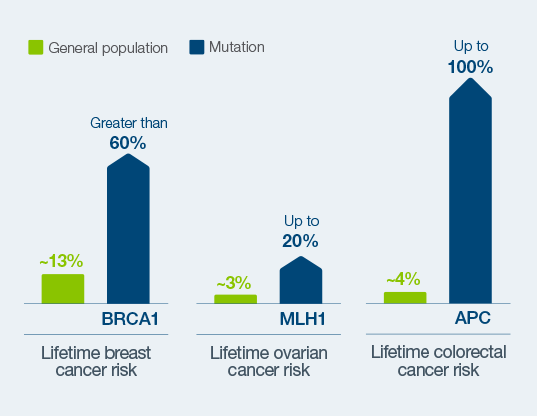
Inherited mutations can significantly increase lifetime risk for developing cancer1
CGA-IGC webinar
GI-cancer case studies:
Utilizing oncologist-initiated testing and the new Natera Hereditary Cancer Alert Program
60 minute webinar
Featured Webinar
[GI-Cancer Case Studies] Capture More Patients & Families Who Can Benefit from Hereditary Cancer Testing: Utilizing the Natera Hereditary Cancer Alert Program and Oncologist Initiated Testing
Join Dr. Shruti Singh, Medical Oncologist / Hematologist at Northwest Cancer Centers, Natera and CGA IGC for a 60-minute webinar to discuss how providers in the Oncology clinic can initiate hereditary cancer testing through the new Natera Hereditary Cancer Alert Program to capture more patients who can benefit from genetic information.
Webinar Objectives:
- Explore how to implement oncologist / clinician initiated hereditary cancer testing into workflows and the resulting impact on patient outcomes
- Learn how the new Natera Hereditary Cancer Alert Program (HCAP) works to help identify more patients who meet testing guidelines in Oncology clinics
Learn More About Genetic Mutations & Hereditary Cancers
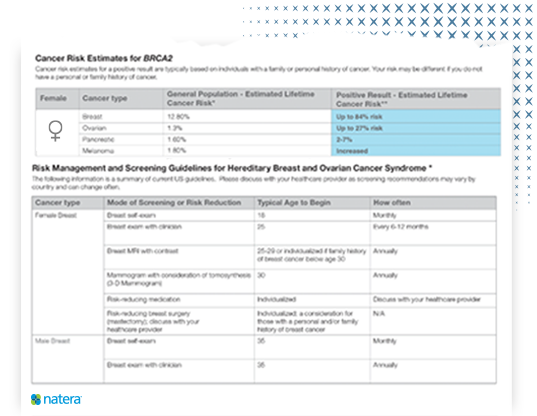
Hereditary Breast and Ovarian Cancer (HBOC) Syndrome
Up to 10% of all breast cancers can be attributed to hereditary causes, the most well known of which is a BRCA1 or 2 mutation. Inherited mutations can increase a woman’s risk for breast cancer to greater than 60%1, yet up to 97% of women who carry that risk don’t know it.2 Patients who know their hereditary or familial cancer risk have better outcomes than those who don’t.3
“Had I known that I carried the BRCA1 mutation when I was first diagnosed, I would have had the opportunity for different treatment options. It’s an important lesson for providers – talk about family cancer history.”
AMY V. – BRCA1 mutation carrier, breast cancer survivor
Lynch Syndrome
As many as 1 in 370 people are Lynch syndrome carriers,4 yet 95% of them do not know.5 Lynch syndrome is the most common inherited cause of colon cancer and endometrial cancer. In fact, gynecologic cancer is a hallmark of Lynch syndrome. Early identification of Lynch syndrome can help manage cancer risk.5,6,7,8
“I feel like the luckiest person in the world to have this information. I can be a previvor. I can take control of my health now and make sure that I don’t ever have to deal with uterine or colon cancer like every woman in my maternal line has so far.”
JENNIFER PLENT – Lynch syndrome mutation carrier, cancer previvor
How it works

Provider orders an Empower Hereditary Cancer Test.

Patient provides a blood or saliva sample.

Patients review results with their provider in about 2 weeks.
Actionable reports guide next steps, including:
- Detect cancer at its earliest, most treatable stage
- Identify risk-reducing medications and surgeries
- Inform surgical and therapeutic decisions following a cancer diagnosis
- Notify family members to help them proactively manage hereditary cancer risk
Making the difference for families with hereditary cancer
“Our mom isn’t here to walk us through this journey.” Hannah and Katie made proactive health plans together after learning they carry a BRCA1 mutation.
NEVA, Natera Educational Virtual Assistant
- Streamlined family cancer history intake
- Interactive results delivery and genetic education, available 24/7
Is Empower right for you? Contact us.
References
1NCCN Guidelines Genetic/Familial High-Risk Assessment: Breast, Ovarian, and Pancreatic Cancer v.3.2023
2Knerr S, et al. Trends in BRCA Test Utilization in an Integrated Health System, 2005-2015. J Natl Cancer Inst. 2019 Aug 1;111(8):795-802. doi: 10.1093/jnci/djz008. PMID: 30753636; PMCID: PMC6695306.
3Domchek SM et al. Association of risk-reducing surgery in BRCA1 or BRCA2 mutation carriers with cancer risk and mortality. JAMA. 2010 Sep 1;304(9):967-75. doi:10.1001/jama.2010.1237. PMID: 20810374; PMCID: PMC2948529.
4Hampel H, de la Chapelle A. “How do we approach the goal of identifying everybody with Lynch syndrome?” Familial Cancer, Jun. 2013, https://pubmed.ncbi.nlm.nih.gov/23568035/.
5Lowry, Blue Ribbon Panel Report. 2016. https://www.cancer.gov/research/key-initiatives/moonshot-cancer-initiative/blue-ribbon-panel#ui-id-3
6Cancer.net editorial board. “Lynch Syndrome.” Cancer.Net, 11 Aug. 2021, https://www.cancer.net/cancer-types/lynch-syndrome.
7Surveillance, Epidemiology and End Results (SEER) Program (https://seer.cancer.gov/)
8Rubenstein JH et al. American Gastroenterological Association Institute Guideline on the Diagnosis and Management of Lynch Syndrome. Gastroenterology. 2015 Sep;149(3):777-82; quiz e16-7.f