Prospera-powered monitoring for any transplant patient
Who is being missed?
Every patient has a unique and complex set of risks for transplant rejection. Surveillance testing with Prospera can have a positive impact for any patient risk profile.
Regularly scheduled testing with Prospera identifies out-of-baseline trends that may indicate larger transplant issues, enabling physicians and patients to quickly tailor healthcare with the most current data. And, Prospera’s simple blood draw can be run along with other labs, limiting patient inconvenience while maximizing peace of mind.
Let’s check out how Prospera provides different benefits based on the varying complexities of each patient.

Key Clinical Factors to Consider when Assessing for Transplant Rejection
| DONOR-SPECIFIC ALLOANTBODY (DSA) DETECTED | HISTORY OF REJECTION | NON-ADHERENCE OF ANTI-REJECTION MEDICATION | HIGH CALCULATED (CPRA) | DELAYED GRAFT FUNCTION (DGF) OCCURENCE | DECREASED IMMUNE SUPPRESSION DUE TO INFECTION AND/OR ADVERSE EFFECTS | GEOGRAPHIC DISTANCE OR ACCESS TO TRANSPLANT CENTER |
|---|---|---|---|---|---|---|
Meet our Prospera patients

Meet Mary, 31, African American
Through Mary’s case, learn how Prospera can identify the need for a biopsy and lead to a change in treatment.
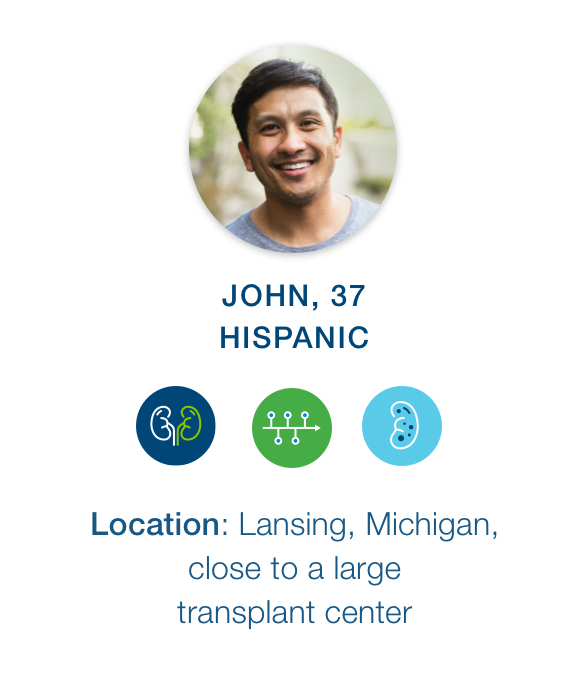
Meet John, 37, Hispanic
Through John’s case, learn how Prospera can help limit unnecessary biopsies.

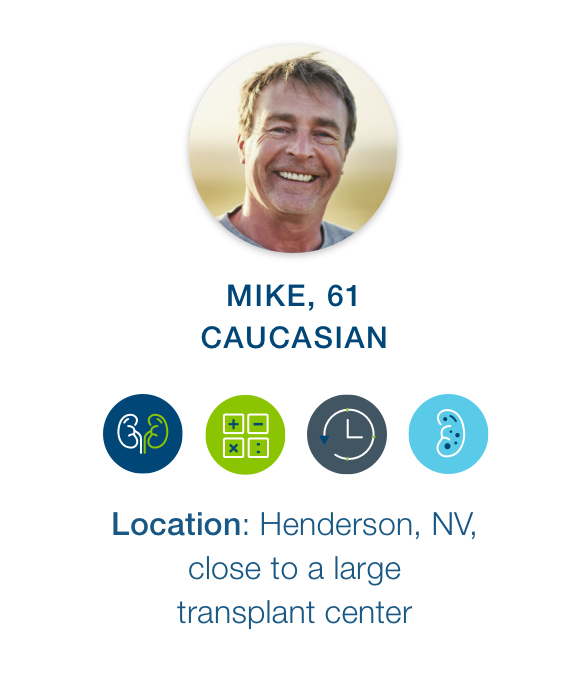
Meet Mike, 61, Caucasian
Through Mike’s case, learn how Prospera can help identify subclinical rejection and allow for earlier treatment.
Meet Mary
| PATIENT | CLINICAL NOTES | KEY TAKEAWAY |
|---|---|---|
 |
|
Prospera surveillance testing allowed Mary’s doctor to closely track drastic fluctuations from the baseline result, which served as an early warning that something more problematic may soon occur. The subsequent results led to a confirmatory biopsy and a modification in treatment — which ultimately may have saved the graft in this complex patient. Download Mary’s case study to learn more details about her clinical results. |
Meet John
| PATIENT | CLINICAL NOTES | KEY TAKEAWAY |
|---|---|---|
 |
|
Prospera surveillance testing allowed John’s doctor to closely track drastic fluctuations from the baseline result, which served as reassurance even though the Cr levels were rising. After a potentially unnecessary biopsy in January 2021, the physician determined the future biopsies may be avoidable when Prospera results are available to supplement fluctuating Cr results due to Prospera’s strong negative predict value. Download John’s case study to learn more details about her clinical results. |
Meet Mike
| PATIENT | CLINICAL NOTES | KEY TAKEAWAY |
|---|---|---|
 |
|
Monitoring kidney transplant recipients with Prospera may help identify subclinical rejection and allow for earlier treatment instead of relying on serum creatinine alone. Download Mike’s case study to learn more details about his clinical results. |